By Ali Weatherford in consultation with Belinda Rico
(Trigger warning: discussion of prematurity and NICU stays)
A NICU is a Neonatal Intensive Care Unit. These special units in the hospital are for newborn babies who need some extra care. Not all hospitals have a NICU, and they also come in different levels. No parent hopes that their newborn needs time in the NICU, but it happens. Fortunately, most of the time, a NICU stay is recommended because a baby needs a little bit of extra support but is overall healthy.
NICU Levels Explained
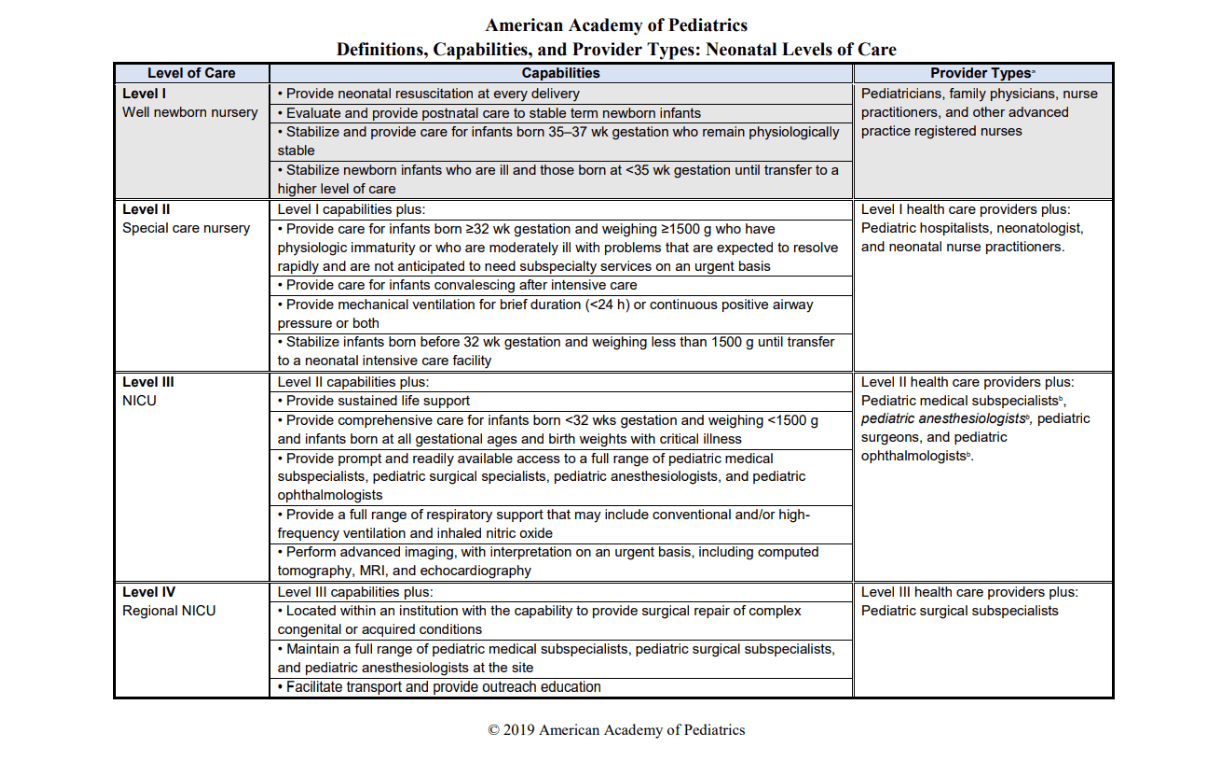
Most hospitals have either a Level 2 or Level 3 NICU. That means that they can support babies who are born prematurely, or have another condition that means they need extra support before they’re ready to go home. A level 3 NICU can support very early preemies or sick and fragile babies, but they might also have very healthy full term newborns who just need a little help regulating their blood sugars or to be treated for jaundice. If you are pregnant and in a situation where you know your baby is at high risk for needing high level NICU care, you might want to learn about the NICU at your hospital. The table below shows more detail about what the NICU levels mean.
Adjusting Expectations
NICU stays usually come as a surprise, and many parents feel overwhelmed and anxious when they’re told their baby needs to transfer to the NICU. Most parents feel shocked and don’t know what to do or what to expect. You probably had visions of what it would be like to meet your baby for the first time, and a NICU stay means you have to be separated and you don’t get to have your vision realized. You may not get to have that “Golden Hour” with your new baby that you were hoping for. You will have to adjust your expectations, but that can be so hard. When plans change, know that you can still find ways to connect with your baby. There are still things that you can do to provide for your baby and be there for them.
A Day in the NICU
The birth parent will still be a hospital patient, and in most cases, will be in a different part of the hospital. Some NICUs now have private rooms where parents and babies can stay together, but most of the time, the birth parent will stay in the postpartum room until they are discharged. This separation can be very difficult. Parents can visit their babies, but for the birth parent, it means having to get out of bed and get help to get there. It’s a good idea for parents to have a conversation about how they might want to handle a NICU stay. If Mom can’t get to the NICU right away, should Dad go to be with the baby? With smart phones, you can have a video call to stay in touch that way. Later, both parents will be able to visit with their baby.
By most accounts, NICU nurses, lactation consultants, and staff members are especially compassionate and accommodating. Parents are usually encouraged to be at their baby’s side whenever they want. When the baby is stable enough, you may even be encouraged to hold your baby skin-to-skin. Both parents can provide this kind of care. There is plenty of evidence showing the benefits of skin-to-skin care for even very fragile newborns in the NICU. Breastfeeding rates and breastmilk supply are improved, the baby’s vital signs can improve, and it’s even associated with improved neurodevelopment as the baby matures. The NICU staff can help you do this safely. They understand that you are going through a very difficult time and you might feel nervous about holding your baby. They also understand that your baby benefits from having you close.
So you might be holding or touching your baby, or just being there next to your baby. Some parents spend the day at their baby’s bedside while reading or watching TV or even getting some work done. Some parents spend time pumping milk for their baby at the bedside. A lot of parents feel they are most successful with pumping when they can be close to their baby
Once the birth parent is discharged from the hospital, they may spend more or less time in the NICU depending on how they feel and their circumstances. It also might depend on the type of NICU available. If the baby has a private room and a bed is provided for parents, some parents choose to spend most of their time at the hospital.
A nurse will probably teach you about your baby’s basic care needs and even encourage you to help with their care. Most NICUs also have a lactation consultant on staff who can help you with your feeding goals.
Breastmilk in the NICU
Breastmilk is great for all babies, but it’s especially beneficial for premature and sick babies. Milk Banks collect donor human milk with the primary goal of supplying NICUs with human milk as medicine for the most vulnerable babies. Breastmilk can mean the difference between life and death for these fragile babies. While any human breast milk is medicinal for these babies, your own milk is actually even a step above. It is especially designed to meet your baby’s very specific needs. You might be able to give your baby breastmilk directly from your breast right away, but that’s unusual in the NICU. Most often, babies are too small or weak or sick to do that. It takes a lot of energy and strength to get milk from a breast. There are many ways to give babies breastmilk:
- Gavage feeding: When babies are very small and the concern is getting them to grow, it’s important that they not burn any more calories than absolutely necessary. In this case, babies are fed breastmilk through a gavage so they don’t have to suck and swallow, burning precious calories. Gavage feeding is when they insert a very small tube into the baby’s nose and feed it down all the way into the baby’s stomach. The milk is pushed through the tube using a syringe. A registered dietician calculates the amount of milk needed for your baby to grow.
- Gavage feeding at the breast: Once a baby is strong enough to do a little work, they might be given their gavage feeding at the breast. The baby is encouraged to smell and touch and lick the breast while the milk is pushed into the tube. They can start to associate the feeling of a full belly with being at the breast and can more easily graduate to direct breastfeeding that way.
- Combination feeding: A baby might still get fed through the gavage, but may also be encouraged to try direct breastfeeding or bottle feeding for some snacks or meals. Sometimes, a baby might even get small amounts of breastmilk from a sponge, cup, spoon, or syringe.
- Bottle feeding: It’s important not to let a baby become too comfortable drinking from a bottle, so a slow-flow nipple is usually tried first. The baby has to do some work to get the milk out, making it more similar to breastfeeding. You may also learn how to position your baby so that the milk in the bottle doesn’t come out too quickly. A lactation consultant might teach you to feed your baby in a side lying position.
Exclusive Breastfeeding
The goal in the NICU is to get the baby feeding at the breast as often as possible. Most babies leave the NICU before they are at the point of exclusive breastfeeding. Most of the time, babies leave the NICU getting some or even most of their milk from the breast, but are still supplementing with pumped milk, donor milk, or formula in a bottle. It’s very possible to continue to increase the amount of milk your baby gets directly from the breast until supplementation is no longer needed. Some families struggle to do this. It can be hard to imagine changing something that’s working, so it’s important to get some support from a lactation consultant outside of the hospital. With a little help, many babies graduate from the NICU and go on to breastfeed exclusively.
Lactation Consultant in the NICU
A lactation consultant should visit with you to talk about your options for feeding your baby and provide support along the way. This will usually be a lactation consultant who works primarily in the NICU. They have some special knowledge and skills for helping these special babies and families achieve their breastfeeding goals. On the first day, you’ll probably get some good education about breastmilk, and how you might be able to provide it for your baby. The consultant might get you a hospital grade pump and get you started on a schedule for pumping. The milk you pump can be given to your baby immediately, but it’s also important to pump on a specific schedule so that you continue to make milk and develop a good milk supply. Most of the time, you’ll pump on a schedule similar to how a newborn baby would eat at the breast. They usually recommend pumping at least 8 times a day, with at least one of those sessions being in the middle of the night or VERY early morning, just like a newborn would do.
If your baby is strong enough to breastfeed directly, your lactation consultant can assess that and help you get started.
If your goal is to eventually breastfeed exclusively, there are ways to start introducing the breast so that your baby can get familiar with it and practice some of the skills they’ll eventually need to breastfeed. A lactation consultant can give you all the tools and support you’ll need to meet your goals. Even more than that, a lactation consultant can be a counselor and even a friend.
The NICU staff may come to feel like a second family. They are usually very compassionate and supportive. They are there because they love to help these tiny babies grow and thrive. They understand how the parents are likely feeling, and they want to make you feel included as part of your baby’s care team and become the leader of that team. They want to help you feel empowered to feed and take care of your baby so you feel ready to go home and do it on your own. It’s important to listen and participate while your baby is in the NICU.
Benefits of Breastfeeding
The benefits of breastmilk to the babies are very clear. It’s medicine. It helps them heal, grow, digest food effectively, and fight off infections. Providing breastmilk can also have benefits for parents. It can be psychologically very difficult to be the parent of a NICU baby. As the birth parent, you’ll be doing your own physical recovery on top of your worries and concerns for your baby’s well-being. You might feel afraid, exhausted, overwhelmed, confused, lost, and even guilty. You might worry that you did something wrong, and that it’s your fault that your baby is in the NICU. These are all very normal feelings. It is not your fault, but you do have the ability to help. It might not feel like it at first. There is a big staff of qualified health care professionals looking after your baby, but they can’t do everything.
For many mothers, pumping breastmilk for their babies from their own recovery room is a way to feel helpful, and is extremely helpful, even vital. Especially when parents can’t be with their babies, it can feel very empowering to provide them with the milk they need to get stronger. Then when you’re with your baby, having skin-to-skin time and learning to breastfeed together, you’re giving them, and yourself, even more strength and comfort.
Benefits of Support
Having a baby in the NICU can be one of the most challenging situations in a person’s life. You need support. In addition to the staff and your own support network of family and friends, most NICUs have peer support groups that they can put you in touch with. Hand to Hold is the group that provides services for NICU families in my local hospital. These volunteers are often former NICU parents who understand the difficulties and special needs of the parents who are caring for babies in the NICU. You may find a lot of comfort in talking to these parents and even other current NICU parents.
As hard as it is to have a baby in the NICU, it’s great to remember that most of the babies leave healthy and strong and go on to live long and productive lives. NICU parents also become stronger and wiser having gone through that experience so early in their parenting. There’s a lot of sadness and hardship in the NICU, but there is also a lot of joy and celebration.
Resources
Skin-to-skin ‘kangaroo care’ found to boost neurodevelopment in preemies

