Ali Weatherford
Co-sleeping or bed sharing is an extremely controversial topic that often leaves families without a clear answer. Everyone wants to keep their babies safe and happy, but finding that balance isn’t always easy!
First, it’s important to understand the difference between co-sleeping and bed sharing. Co-sleeping can mean bed sharing, but can also just mean sharing a room. That’s usually what the medical professionals mean when they say that co-sleeping is recommended for the first six months to one year. Bed sharing means your baby is in the bed with you, and this can be done more or less safely. Here are some different ways that people co-sleep or bed share:
- Baby is in your bed sharing the same sleep surface. You and your baby are on the same mattress, bedroll or mat.
- Baby is in your bed but on their own sleep surface. There are small baby beds or baskets that are designed to be put right next to you in your bed.
- Baby is in a bassinet or co-sleeper right next to your bed or even connected directly to it. They usually have some storage for supplies like spare sheets and diapers that you might need in the middle of the night so you don’t have to go far to attend to your baby.
- The co-sleeper may have a wall or rail all the way around it. The baby needs to be lifted in and out. A co-sleeper is designed to be attached to an adult bed or butt up right against it.
- The co-sleeper may attach securely to your bed and have a side that drops so the baby can be easily rolled or scooted in and out for feeding or other night time care.
- A bassinet is a standalone baby bed. It’s like a crib but much smaller and easier to move around
- Baby is in a crib or bassinet farther away from your bed but in the same room. In this situation, you would need to get out of bed to attend to the baby.
What is the recommendation?
Put simply, the recommendation from the American Academy of Pediatrics (AAP) is that adults DO share a room with their babies for at least the first six months and preferably for the first year of life. Sharing a room provides a measure of safety and convenience for families. The recommendation is also that adults don’t share a sleep surface with their babies. These recommendations get a little more complex as you keep digging, though. There are some exceptions to this advice and there should also be some EXTRA recommendations to think about to ensure that it’s safe. For example, if there is a smoker in the room, you need to weigh that into your decision making because that increases risks to babies.
Also, if your baby needs to be fed, and you feel like you are at risk for falling asleep, it’s best to get in your bed to feed your baby. The AAP says specifically, “The AAP acknowledges that parents frequently fall asleep while feeding the infant. Evidence suggests that it is less hazardous to fall asleep with the infant in the adult bed than on a sofa or armchair, should the parent fall asleep.”
Basically, it’s much safer to fall asleep with your baby in a safe bed rather than on the couch or in a rocker or other chair. It’s important to learn safe sleep guidelines, whether your baby sleeps in your bed or in their own. If your baby is at high risk because of prematurity or other conditions, it’s especially important to offer only safe sleep options. Most sleep-related infant deaths occur in higher risk babies, and/or on unsafe sleep surfaces like couches, armchairs, or in beds that are not baby-proofed.
What are people worried about specifically?
Sudden Infant Death Syndrome (SIDS) is usually referred to as the main concern when discussing safe sleep. This very devastating condition used to be called Crib Death or Cot Death. SIDS can happen anywhere, even when babies are alone in a crib or “cot” and there are no barriers to safe sleep. More and more evidence points to the idea that SIDS is caused by a baby’s inability to wake up or arouse from a deep sleep. Their breathing deepens and slows to the point of almost stopping, but when this happens they don’t wake up to take a deep breath like people usually do.
That’s why having things in their sleep environment that can keep the baby from sleeping too deeply are important, such as sharing a room with their parents. The movements and sounds of other people in the room can keep them from sleeping too deeply. Also, newborn baby bellies are designed to be very small, and breast milk digests very quickly, so waking often because of hunger helps keep a baby from sleeping too deeply. That’s why exclusive breastfeeding is associated with lower rates of SIDS.
Normal healthy newborn sleep patterns also keep babies waking often. That offers protection against SIDS. Newborns especially should not be expected or forced to “sleep through the night”. This might be really frustrating for parents, BUT protective for babies!
Sleep related infant deaths: SIDS vs SUID
It’s most often the case that SIDS is the only sleep related cause of infant death that is mentioned to parents. There is definitely misinformation and some confusion, so SIDS tends to get lumped in with other causes of infant death during sleep which can include smothering, falling, wedging or other accidents.
The actual definition of SIDS is:
“The sudden death of a baby younger than 1 year of age that doesn’t have a known cause, even after a full investigation.”
There is another term, Sudden Unexpected Infant Death or (SUID). The definition of SUID is:
“An umbrella category that describes all sudden, unexpected infant deaths—those from known causes, such as an injury or accident, and those from unknown causes.”
So, while SUID is definitely more often associated with bed sharing, SIDS may not be, or at least not as much.
This means that the risks of bed sharing are more about accident and injury or KNOWN causes of infant death, SUID not SIDS.
Why does this matter?
It’s thought that the actual number of families who share a bed with their babies is MUCH higher than reported. Most statistics report that somewhere between 24-30% of families tell their pediatricians that they bed share, but the actual number of families who reported bed sharing in a frequently cited 2015 study was 61%. The actual number today is likely even higher than that.
Most people who are bed sharing do it in secret. There is shame associated with bed sharing because of all the public service announcements and physician recommendations against it, and they don’t want anyone to know. This is very unfortunate and might even be contributing to higher risk for babies. When people feel free to tell their care providers about their sleeping needs, they can get information about how to lower their risks for accidents and infant death. Unfortunately, most people are not getting the information they need to find better options, or make bed sharing a safer solution for their family.
The question of nature
It is very natural for parents and babies to want, or even need, to sleep together. There are many studies showing benefits to closeness during sleep, specifically between babies and the breastfeeding parent. It’s the way babies were designed to be parented and fed at night. Bed sharing is also associated with higher breastfeeding rates and longer duration of breastfeeding. We know that breastfeeding is associated with other types of risk reduction. The problem is not necessarily just the practice of sharing sleep, but more about the circumstances that many modern families find themselves in for sleeping. Beds are too soft and too high off the ground. Many parents take medication or use alcohol or other recreational drugs. People fall asleep with their babies on couches or in baby rockers.
It’s critical to avoid accidental bed sharing
The riskiest type of bed or sleep surface sharing is when parents fall asleep with their babies without intending to, and without preparing to do it most safely. Remember that the AAP includes a recommendation to help prevent this.
– “The AAP acknowledges that parents frequently fall asleep while feeding the infant. Evidence suggests that it is less hazardous to fall asleep with the infant in the adult bed than on a sofa or armchair, should the parent fall asleep.”-
However, there should be additional education to go along with this recommendation to be even safer. Parents should also be educated about ways to make their beds a safer place to fall asleep with their babies, EVEN WHEN THEY DON’T INTEND TO. The AAP provides this table in the most recent publication. The University of Notre Dame provides this checklist to help parents.
For your breastfeeding relationship
Breastfeeding Success is a team of lactation consultants (IBCLCs) and other breastfeeding and perinatal professionals with the goal of educating and supporting new families. We want you to have all the information you need to make informed decisions that are right for YOUR family. We also work hard to protect breastfeeding for the families that choose it, and that sometimes means offering useful and evidence based information on a number of topics including medication use, nutrition, sleep, and even clothing choices! We uphold research and empowerment with knowledge.
Our company even provides a stipend for continuing education for all of our staff members whether part or full time, and we also offer an Infant CPR & Safety class for families which provides education on a number of topics related to your baby’s safety. Some concepts related to infant sleep and breastfeeding that are backed by evidence include:
- SIDS rates are lower in breastfed infants, especially when exclusively breastfeeding.
- Frequent feedings, including nighttime feedings, are very important for milk supply and infant development and should not be restricted, especially for newborns.
- Closeness between the breastfeeding parent and newborn is important for milk production and successful breastfeeding outcomes. When you can keep nighttime feedings quick and easy, it won’t be as hard to maintain. When your baby is within arms reach, you can minimize disruptions to everyone’s sleep, and even keep the lights off.
- Remember that “topping off” a newborn with a bottle before going to bed at night using formula or cereal so they will sleep longer or more deeply is not recommended. It’s safer for SIDS prevention that the baby sleeps less deeply, and it’s better for establishing your milk supply that the baby feeds more often.
- When you need to feed your baby in the bed, a helpful tip might be to set a quiet alarm for yourself so you can wake up and move your baby if you fall asleep.
- When you need to feed your baby in the bed, it can be done more safely by following some safe sleep guidelines:
- A mattress on the floor is best to minimize the risk of falling.
- The mattress should not be against a wall or have any barriers around it that a baby could get wedged between.
- The mattress should be firm and flat.
- The baby should be on their back.
- No one in the room should be smoking or vaping.
- Anyone sharing the bed should be a sober, consenting, and responsible adult.
- Large or heavy blankets, excess pillows, and any other objects should be removed from the bed.
- Light blankets or sheets might be used but should never cover the baby completely.
- Baby should be full term and healthy.
- No swaddles or tight wraps.
- Direct breastfeeding minimizes risks. Bottle feeding increases risks for bed sharing accidents.
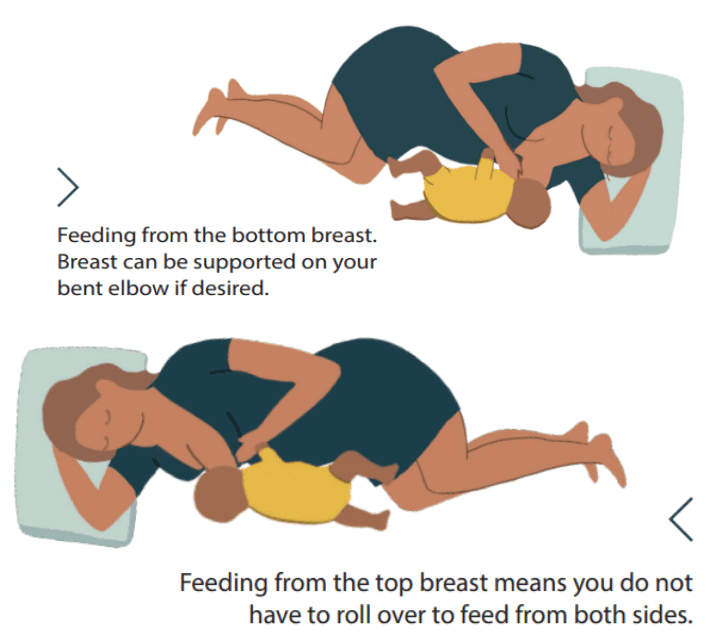
- The best position for the breastfeeding parent is:
However you choose to parent your baby at night, it’s best to learn about your options and about how to proceed safely. You should never be made to feel wrong or irresponsible, but instead should be offered information and options. Breastfeeding Success strives to be a great source of information and support for new families. You can take a class with us, see one of our lactation consultants, or join one of our FREE new parent groups.
Resources
Healthy Children.org – a publication of the AAP
Updated publication by AAP – 2022 – includes safe sleep recommendations table
Durham University Infancy and Sleep Centre
Basis (Baby sleep info source) – a publication of the Durham University Sleep Centre
Where Babies Sleep (A Basis publication)
Normal Infant Sleep Development (A Basis publication)
Mother-Baby Sleep Lab – University of Notre Dame
Safe Co-sleeping Guidelines – Posted by Mother-Baby Sleep Lab of Notre Dame
The Lullaby Trust – safer sleep advice
Academy of Breastfeeding Medicine Infographic for safe sleep
Academy of Breastfeeding Medicine Infographic for supporting breastfeeding and sleep

